Anti-Inflammatory Diet for Brain Health: The Evidence-Based Nutrition Protocol
Medical Disclaimer: The information in this article is for educational purposes only and does not constitute medical advice. Dietary changes for the management of health conditions require consultation with a qualified healthcare provider or registered dietitian. Food allergies, intolerances, and medication interactions with specific foods require professional evaluation. Individual responses to dietary changes vary significantly.
The brain consumes approximately 20% of the body’s total energy despite comprising only 2% of its mass — and every calorie that powers neural activity, every molecule that makes up a synaptic membrane, every precursor that the brain synthesizes into a neurotransmitter comes from what you eat. The idea that diet affects brain function is not a claim that needs to be argued for — it is a straightforward consequence of biochemistry. What the research has clarified over the past two decades is which specific dietary factors affect which specific neurobiological mechanisms, and with what magnitude across which timescales.
The answer centers on inflammation. Chronic low-grade neuroinflammation — the persistent activation of the brain’s immune cells in response to dietary, metabolic, and lifestyle inputs — is now recognized as the central mechanism underlying most forms of age-related cognitive decline, Alzheimer’s disease, depression, and the diffuse cognitive slowing that most adults experience through midlife. The foods and dietary patterns that drive systemic inflammation cross the blood-brain barrier and activate the microglial neuroinflammatory signaling that impairs synaptic plasticity, reduces hippocampal neurogenesis, disrupts memory consolidation, and accelerates the amyloid-beta accumulation that precedes Alzheimer’s pathology. And the foods that reduce systemic inflammation produce the opposite: reduced microglial activation, improved neuroplasticity, better cognitive aging trajectories.
This is the final article in the Brain Health hub — completing the neuroprotective framework that the brain health pillar guide, neuroplasticity guide, cognitive decline prevention guide, and neuroprotective nootropics guide have established. The dietary protocol here is the nutritional foundation that the supplement stack, sleep optimization, and exercise protocols all operate on — and without which their effects are consistently reduced.
Part 1: How Diet Drives Neuroinflammation — The Mechanisms
Understanding why specific foods harm or protect brain health requires understanding the three pathways through which diet reaches the brain’s immune system.
Pathway 1: Systemic Inflammation Crossing the Blood-Brain Barrier
The blood-brain barrier — the specialized vascular network that controls which molecules enter the brain — is permeable to pro-inflammatory cytokines including TNF-alpha, IL-1beta, and IL-6. When chronic dietary patterns drive systemic inflammation through metabolic dysregulation, gut dysbiosis, or oxidative lipid products, the resulting cytokine elevation crosses the BBB and directly activates microglia — the brain’s resident immune cells. Chronically activated microglia shift from their homeostatic neuroprotective functions to a pro-inflammatory state that impairs LTP induction, reduces BDNF expression, suppresses hippocampal neurogenesis, and releases additional pro-inflammatory signals that further compromise the synaptic environment. Research by Heneka and colleagues established this neuroinflammatory cascade as the central mechanism linking lifestyle factors — including diet — to Alzheimer’s pathology and cognitive aging.
Pathway 2: Gut-Brain Axis Dysregulation
The gut microbiome — the approximately 100 trillion microorganisms inhabiting the gastrointestinal tract — communicates bidirectionally with the brain through the vagus nerve, the enteric nervous system, circulating metabolites, and immune system signaling in what is collectively termed the gut-brain axis. Dietary patterns high in ultra-processed foods, refined carbohydrates, and industrial seed oils produce gut dysbiosis — disruption of the microbial composition that favors short-chain fatty acid-producing bacteria essential for gut barrier integrity and anti-inflammatory immune tone. Dysbiosis increases intestinal permeability (allowing lipopolysaccharide from gram-negative bacteria to enter systemic circulation), shifts the microbiome toward pro-inflammatory metabolite production, and reduces the SCFA output that directly supports the BBB integrity and anti-neuroinflammatory tone that brain health requires.
The dietary patterns that support gut microbiome diversity and SCFA production — high fiber intake, fermented foods, diverse plant foods, adequate polyphenols — are therefore simultaneously gut health and brain health interventions through this axis. The practical implication is that the same dietary pattern that produces gut symptoms (bloating, irregularity, discomfort) is likely also producing gut-brain axis dysregulation with neuroinflammatory consequences — and the dietary changes that improve gut function typically improve cognitive function through the same mechanism.
Pathway 3: Blood Glucose Dysregulation and Advanced Glycation
Chronically elevated blood glucose — from dietary patterns high in refined carbohydrates and added sugars — produces two neurologically damaging effects that accumulate silently over years. First, glucose spikes generate reactive oxygen species and advanced glycation end products (AGEs) that damage cerebrovascular endothelial cells, progressively impairing the cerebral blood flow that neuronal energy metabolism requires. Research on glycemic index and cognitive aging found that higher lifetime glycemic load is associated with accelerated hippocampal atrophy and cognitive decline — with the mechanism involving both direct oxidative damage to cerebral vasculature and insulin resistance in the brain that impairs the insulin signaling required for normal synaptic function. Second, insulin resistance in the brain — now sometimes called “type 3 diabetes” in the context of Alzheimer’s research — impairs the glucose uptake that neurons require for the energy-intensive processes of LTP, memory consolidation, and neuroplasticity. Maintaining stable blood glucose through lower glycemic index food choices is therefore not merely a metabolic health intervention — it is a direct brain health intervention addressing a mechanism that accumulates damage across decades.
Part 2: The Dietary Patterns With Strongest Evidence for Brain Health
The MIND Diet: Designed Specifically for Neuroprotection
The MIND diet — Mediterranean-DASH Intervention for Neurodegenerative Delay — was developed by nutritional epidemiologist Martha Clare Morris specifically by identifying the dietary components most consistently associated with reduced cognitive decline and Alzheimer’s risk in observational research, then combining them into a coherent dietary pattern. Unlike the Mediterranean or DASH diets, which were designed for cardiovascular outcomes and adapted for brain health, the MIND diet was built from the neuroscience outward.
Morris’s landmark research found that high adherence to the MIND diet was associated with a 53% reduction in Alzheimer’s risk over the 4.5-year follow-up period — and even moderate adherence showed a 35% risk reduction. Critically, the MIND diet showed a stronger association with cognitive outcomes than either the Mediterranean or DASH diets applied to the same population, confirming that the brain-specific optimization of its food choices provides incremental neuroprotective benefit beyond general healthy eating patterns.
The MIND diet’s ten brain-healthy food groups: leafy green vegetables (6+ servings per week — the strongest single food category association), other vegetables, berries (2+ servings per week), whole grains, fish (1+ serving per week), poultry (2+ servings per week), beans (4+ servings per week), nuts (5+ servings per week), olive oil as primary cooking fat, and wine (1 glass per day — the most contested element and omittable given alcohol’s sleep REM suppression). The five foods to limit: red meat, butter and margarine, cheese, pastries and sweets, and fried or fast food.
The Specific Foods With the Strongest Individual Evidence
Leafy greens: daily, and non-negotiably. The Morris research found that one serving of leafy greens per day was associated with cognitive aging equivalent to being 11 years younger by the end of the study period — the single strongest food category finding in the entire neuroprotection dietary literature. The active compounds are multiple: vitamin K1 (cerebrovascular protection), folate (homocysteine reduction reducing vascular risk), lutein and zeaxanthin (accumulated in brain tissue where they reduce oxidative stress), and nitrates (converted to nitric oxide that improves cerebral blood flow). Spinach, kale, arugula, Swiss chard, and romaine are the highest-yield options — a daily salad or cooked greens serving is the most impactful single dietary change available for brain health.
Blueberries and dark berries: 2+ servings per week minimum. Anthocyanins — the flavonoid compounds responsible for the dark blue and red pigments in berries — are among the most well-characterized dietary neuroprotectants available. Research by Krikorian and colleagues found that daily wild blueberry supplementation in older adults with mild cognitive impairment produced significant improvements in memory and learning over 16 weeks — with the mechanism involving direct reduction of neuroinflammatory microglial activation and enhancement of hippocampal signaling pathways. Strawberries, blackberries, and cherries provide overlapping but distinct flavonoid profiles that complement blueberry anthocyanins — diversity of berry intake maximizes the flavonoid spectrum.
Fatty fish: 1–2 servings per week minimum. The primary dietary source of DHA — the neuronal membrane lipid that constitutes approximately 40% of brain PUFA content and determines membrane fluidity, LTP induction efficiency, and BDNF receptor sensitivity. As established in the nootropics for brain health guide, DHA deficiency is directly associated with neuroinflammation, reduced hippocampal neurogenesis, and increased dementia risk. Salmon, sardines, mackerel, anchovies, and herring provide the highest DHA per serving — two servings per week provides approximately 500–700mg of dietary DHA, which most people should supplement to reach the 1,000–2,000mg range with the greatest neuroprotective evidence.
Extra virgin olive oil: as primary cooking fat. Oleocanthal — a phenolic compound in high-quality extra virgin olive oil — inhibits the same inflammatory enzymes (COX-1 and COX-2) as ibuprofen, providing direct anti-neuroinflammatory activity at typical dietary doses. Research identifying oleocanthal’s mechanism found that its anti-inflammatory potency at dietary doses is pharmacologically meaningful — not a background effect but a significant anti-inflammatory signal delivered with every use. EVOO additionally provides oleic acid that supports myelin maintenance and hydroxytyrosol, a potent antioxidant that reduces oxidative stress in neuronal tissue. The distinction from refined olive oil and other cooking oils is meaningful — processing destroys the oleocanthal and polyphenol content that provides the neuroprotective effect.
Walnuts: 5+ servings per week. The only nut with significant ALA content (the plant omega-3 that partially converts to DHA), walnuts additionally provide polyphenol-rich membrane material, vitamin E (tocopherols that protect neuronal membranes from oxidative damage), and folate. Research on walnut consumption and cognitive aging found that higher walnut intake was associated with significantly better memory and cognitive flexibility in older adults in two large national health surveys — with dose-response relationships suggesting that more is better within normal dietary ranges.
Free Download
Get the 7-Day Brain Optimization Protocol
The evidence-based diet, sleep, and supplement framework for your first week of cognitive enhancement — completely free.
Join 2,000+ readers optimizing their cognitive performance. Unsubscribe anytime.
Part 3: The Neuroinflammatory Foods — What the Evidence Says to Reduce
The dietary changes that most directly reduce neuroinflammation are not primarily about adding protective foods — they are about removing the dietary drivers of chronic neuroinflammation that are most prevalent in Western eating patterns. The protective foods have additive effects; the inflammatory foods have subtractive effects that undermine what the protective foods are building.
Ultra-processed foods: the highest-priority reduction. Ultra-processed foods — defined by the NOVA classification as industrially manufactured products containing additives, preservatives, flavor enhancers, and ingredients not typically found in home cooking — drive neuroinflammation through multiple simultaneous mechanisms: gut dysbiosis from emulsifiers and artificial sweeteners that disrupt the microbiome, elevated glycemic response from refined carbohydrates that generates oxidative stress and AGE production, high omega-6 to omega-3 ratios that shift prostaglandin balance toward pro-inflammatory eicosanoids, and low fiber content that reduces the SCFA-producing bacteria that support gut barrier integrity. Large-scale epidemiological research found that higher ultra-processed food consumption was associated with significantly faster cognitive decline across all domains measured — with a dose-response relationship suggesting every 10% increase in ultra-processed food proportion of diet was associated with meaningfully accelerated cognitive aging.
Industrial seed oils high in omega-6: the silent neuroinflammation driver. Soybean, corn, sunflower, and safflower oils — the dominant cooking oils in processed and restaurant food — are extremely high in linoleic acid (omega-6), which competes with DHA for incorporation into neuronal membranes and shifts prostaglandin synthesis toward pro-inflammatory pathways. The dramatic increase in omega-6 consumption in Western diets since the mid-20th century has produced an estimated omega-6:omega-3 ratio of 15:1 to 20:1 in typical Western populations, compared to the approximately 4:1 ratio of ancestral human diets and the 4:1 ratio associated with optimal anti-inflammatory prostaglandin balance in the research. Replacing seed oils with extra virgin olive oil and consuming adequate DHA (from fish or supplementation) is the most direct dietary correction for the omega-6-driven neuroinflammatory background that most people in Western food environments carry continuously.
Added sugars and refined carbohydrates: the cerebrovascular damage accumulator. Each glucose spike from refined carbohydrates and added sugars generates an oxidative and glycation insult to cerebrovascular endothelial cells that accumulates across years into the impaired cerebral blood flow and vascular cognitive impairment that represents the second most common dementia mechanism after Alzheimer’s. The practical reduction: replacing refined grain products (white bread, white rice, processed cereals) with whole grain alternatives cuts the glycemic response by 30–50% while adding the fiber that microbiome health requires. Liquid sugars — sweetened beverages including fruit juice — produce the highest glycemic spikes with none of the fiber buffering that whole fruit provides, making them the highest-priority specific item for reduction.
Part 4: The Complete Anti-Inflammatory Brain Health Diet Protocol
🥦 Daily Anti-Inflammatory Brain Health Protocol
DAILY — non-negotiable targets
→ 1+ serving leafy greens (spinach, kale, arugula, romaine)
→ Extra virgin olive oil as primary cooking fat
→ 3+ servings non-starchy vegetables across all colors
→ Whole grains over refined grains at every opportunity
→ DHA 1,000–2,000mg (from fish or supplementation)
WEEKLY — frequency targets
→ 2 servings fatty fish (salmon, sardines, mackerel, herring)
→ 2 servings berries (blueberries, strawberries, blackberries)
→ 5 servings nuts (especially walnuts)
→ 4 servings legumes (beans, lentils, chickpeas)
→ 2 servings poultry; limit red meat to 1–2 servings
MINIMIZE — neuroinflammatory priority reductions
→ Ultra-processed foods (processed meats, packaged snacks, fast food)
→ Industrial seed oils (soybean, corn, sunflower — replace with EVOO)
→ Added sugars and refined carbohydrates (especially liquid sugars)
→ Alcohol (REM suppression, gut dysbiosis, neuroinflammation — limit to ≤1 drink/day maximum)
Practical Implementation: The 80/20 Reality
The dietary pattern matters more than individual meals, and consistent 80% adherence over years produces far better brain health outcomes than perfect compliance for weeks followed by abandonment. The most impactful single implementation decision is environmental: keeping the home food environment aligned with the MIND dietary pattern makes the default choice the brain-healthy choice, rather than requiring active resistance at every meal. When the refrigerator contains leafy greens, berries, olive oil, nuts, and sardines — and the pantry contains whole grains and legumes — the path of least resistance at every meal is the neuroprotective path.
The personal context I apply directly: practicing OMAD (one meal a day), I have found that the quality and composition of that single meal becomes extraordinarily important — and the anti-inflammatory pattern described in this guide is the foundation I have maintained consistently for years. The combination of metabolic benefits from time-restricted eating with the neuroinflammation reduction of MIND-pattern nutrition produces a synergistic effect on both gut-brain axis health and blood glucose stability that neither produces alone. For those not practicing extended fasting, the same principles apply across whatever meal frequency structure you maintain — the food quality matters more than the timing for the neuroinflammation mechanisms this guide addresses.
Frequently Asked Questions About Anti-Inflammatory Diet and Brain Health
What is the best diet for brain health?
The MIND diet — Mediterranean-DASH Intervention for Neurodegenerative Delay — has the strongest specific evidence for brain health outcomes of any dietary pattern studied, associated with a 53% reduction in Alzheimer’s risk in the Morris research with high adherence. It combines elements of the Mediterranean and DASH diets with brain-health-specific optimization of food frequency targets — prioritizing the ten food groups most consistently associated with neuroprotection (leafy greens, berries, fish, olive oil, whole grains, nuts, legumes, poultry) and limiting the five most consistently associated with increased cognitive decline risk (red meat, butter, cheese, pastries, fried food). The neurobiological mechanisms behind the MIND diet’s neuroprotective effects span all three neuroinflammation pathways described in this guide: systemic inflammation reduction (olive oil oleocanthal, berry anthocyanins, fish DHA), gut-brain axis support (high fiber from vegetables, legumes, and whole grains), and blood glucose stabilization (low glycemic index overall structure, replacement of refined carbohydrates with whole food alternatives). The MIND diet is not a calorie-restriction protocol — it is a food quality and pattern protocol that can be implemented across any reasonable caloric level and most cultural food traditions.
Does sugar cause brain damage?
Chronic excessive sugar intake — particularly refined added sugars and liquid sugars — produces measurable neurological consequences through several mechanisms, though “brain damage” requires some nuance. Each significant blood glucose spike generates reactive oxygen species and advanced glycation end products that damage cerebrovascular endothelial cells — the inner lining of the blood vessels supplying the brain. Over years, this accumulated vascular damage impairs cerebral blood flow and produces the white matter lesions associated with vascular cognitive impairment. High sugar intake also promotes the systemic inflammation and insulin resistance that reduce brain insulin signaling — impairing the glucose uptake that neurons require for energy-intensive processes including LTP and memory consolidation. Research on habitual sugar intake and hippocampal function found that higher added sugar consumption was associated with poorer performance on hippocampus-dependent memory tasks and reduced hippocampal responsiveness — with the mechanism involving both direct metabolic effects and elevated cortisol from the glucose-insulin cycling that high sugar intake produces. The practical implication is that added sugars and refined carbohydrates produce cumulative neurological harm through vascular and metabolic mechanisms — not dramatic acute damage but progressive, compounding impairment across years and decades of consistent high intake.
What foods reduce neuroinflammation?
The foods with the strongest evidence for directly reducing neuroinflammation are: fatty fish (salmon, sardines, mackerel) providing DHA that shifts prostaglandin balance toward anti-inflammatory eicosanoids and directly supports neuronal membrane health; blueberries and dark berries providing anthocyanins that directly inhibit microglial pro-inflammatory signaling — with research showing measurable reductions in TNF-alpha and IL-1beta from regular berry consumption; extra virgin olive oil providing oleocanthal with COX-inhibiting anti-inflammatory activity at dietary doses; leafy green vegetables providing vitamin K1, lutein, zeaxanthin, and nitrates that reduce oxidative stress and improve cerebrovascular function; and walnuts providing ALA, vitamin E tocopherols, and polyphenols with combined antioxidant and anti-inflammatory effects. The foods that most directly increase neuroinflammation — and whose reduction produces the largest neuroinflammatory benefit — are ultra-processed foods, industrial seed oils high in omega-6, and refined carbohydrates that produce glucose spikes and AGE formation. The most effective single dietary intervention for neuroinflammation reduction is replacing industrial seed oils with extra virgin olive oil across all cooking and dressing applications — it simultaneously removes the primary dietary pro-inflammatory lipid and replaces it with the dietary compound with the strongest individual evidence for anti-neuroinflammatory effect.
How quickly does diet affect brain function?
Diet affects brain function across multiple timescales simultaneously — some effects are visible within hours, others require months or years. The fastest dietary effects on cognition occur within hours: glucose spikes impair working memory and attention within 30–60 minutes of consumption through the insulin dysregulation and subsequent hypoglycemic rebound that follows rapid glucose absorption, while a high-fat, high-sugar meal can impair cognitive function measurably for the 2–3 hours following it through inflammatory signaling and reduced cerebral blood flow. Within days to weeks, dietary shifts that reduce inflammation and stabilize blood glucose typically produce noticeable improvements in energy consistency, mental clarity, and mood — reflecting gut microbiome compositional changes beginning within 3–5 days of consistent dietary change and early systemic inflammation reduction. The most significant neuroplasticity effects — changes in hippocampal neurogenesis rates, synaptic density, and cognitive reserve — develop over months of consistent dietary pattern adherence, paralleling the timelines of the structural supplementation compounds in the neuroprotective stack. And the most important brain health effects of diet — reduced amyloid-beta accumulation, maintained hippocampal volume, lower Alzheimer’s risk — are measured in years and decades of consistent eating patterns, not weeks. The practical implication: dietary changes produce some immediate cognitive benefits, meaningful medium-term improvements, and the most important long-term neuroprotective effects — all of which are relevant and all of which require sustained application of the same pattern.
Diet as the Foundation Everything Else Rests On
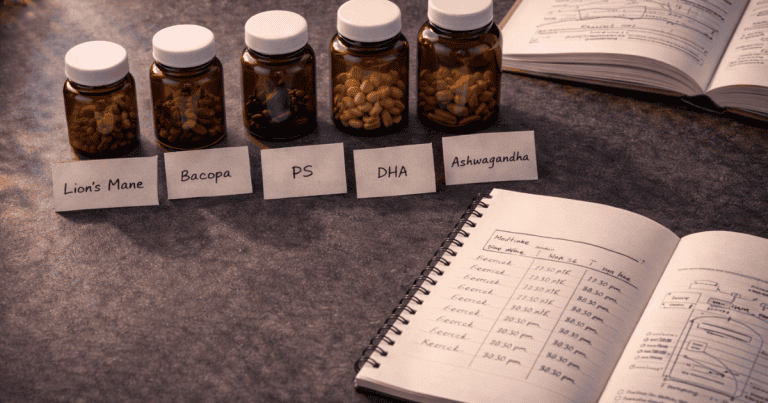
The supplement stack from the nootropics guide and the sleep optimization from the Sleep hub are more effective when the dietary foundation supports rather than undermines them. Lion’s Mane’s NGF stimulation operates more effectively in a brain with adequate DHA membrane fluidity. Bacopa’s antioxidant protection is more complete when dietary polyphenols are simultaneously reducing the oxidative burden it needs to address. Magnesium L-Threonate’s NMDA optimization is more consequential when blood glucose stability allows neurons to respond to NMDA-mediated plasticity signals without the metabolic interference of insulin resistance. The supplements amplify what the diet builds — they do not substitute for it.
After 18+ years of observing what actually moves the needle in cognitive performance and brain health, the pattern is consistent: the individuals who achieve the most significant and durable improvements are those who address the dietary foundation first, then stack the behavioral and supplementation protocols on top of a stable nutritional substrate. The MIND pattern is not a difficult diet — it is the way humans evolved to eat, with modern nutritional science identifying precisely which elements of that pattern most directly address the specific mechanisms of neurobiological aging. Implement it as a permanent pattern rather than a protocol, and it becomes the background against which everything else in NeuroEdge Formula becomes more effective.
This article completes the Brain Health hub. For the complete neuroprotective context, return to the brain health pillar guide. For the nootropic compounds that work synergistically with this dietary foundation, see the neuroprotective nootropics guide. For the sleep optimization that completes the neuroprotective triad, see the Sleep hub.
References
- Morris, M.C., et al. (2015). MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimer’s & Dementia, 11(9), 1007–1014. PubMed
- Heneka, M.T., et al. (2015). Neuroinflammation in Alzheimer’s disease. The Lancet Neurology, 14(4), 388–405. PubMed
- Krikorian, R., et al. (2010). Blueberry supplementation improves memory in older adults. Journal of Agricultural and Food Chemistry, 58(7), 3996–4000. PubMed
- Beauchamp, G.K., et al. (2005). Phytochemistry: Ibuprofen-like activity in extra-virgin olive oil. Nature, 437(7055), 45–46. PubMed
- Sala-Vila, A., et al. (2022). Dietary marine omega-3 fatty acids and incident sight-threatening retinopathy. JAMA Ophthalmology, 140(8), 750–758. PubMed
- Arab, L., & Ang, A. (2015). A cross sectional study of the association between walnut consumption and cognitive function. Journal of Nutrition, Health and Aging, 19(3), 284–290. PubMed
- Schnabel, L., et al. (2019). Association between ultraprocessed food consumption and cognitive decline. JAMA Neurology, 76(5), 519–528. PubMed
- Gu, Y., et al. (2010). Mediterranean diet and brain structure in a multiethnic elderly cohort. Neurology, 75(14), 1195–1202. PubMed
- de Lau, L.M., et al. (2005). Dietary fatty acids and the risk of Parkinson’s disease: The Rotterdam study. Annals of Neurology, 58(2), 310–314. PubMed
- Gomez-Pinilla, F. (2008). Brain foods: The effects of nutrients on brain function. Nature Reviews Neuroscience, 9(7), 568–578. PubMed
Tags: anti-inflammatory diet brain health, MIND diet, brain healthy foods, neuroinflammation diet, foods that reduce neuroinflammation, blueberries brain health, leafy greens cognitive decline, DHA brain health diet, olive oil brain health, omega-3 brain health, gut brain axis diet, blood glucose brain health, ultra-processed foods cognitive decline, MIND diet Alzheimer’s, brain health nutrition protocol
About Peter Benson
Peter Benson is a cognitive enhancement researcher and certified mindfulness coach with 18+ years of personal and professional experience in nootropics, neuroplasticity, and brain health optimization. He practices OMAD (one meal a day) and has extensive firsthand experience with the cognitive effects of dietary pattern changes. NeuroEdge Formula is his platform for sharing rigorous, safety-first cognitive enhancement guidance.