HRV Training and Stress Optimization: The Science of Autonomic Performance
Medical Disclaimer: The information in this article is for educational purposes only and does not constitute medical advice. HRV measurement and biofeedback are generally safe, but individuals with cardiac arrhythmias, pacemakers, or other cardiovascular conditions should consult a qualified healthcare provider before using HRV monitoring devices or biofeedback training. HRV data should not be used to self-diagnose medical conditions. Always consult a qualified healthcare provider for cardiovascular health concerns.
Heart rate variability — the millisecond-to-millisecond variation in time between consecutive heartbeats — is the most information-dense single biomarker available from consumer health monitoring devices. A high HRV does not mean the heart is beating irregularly or erratically. It means the autonomic nervous system is functioning with the flexibility and responsiveness that health and cognitive performance require — efficiently shifting between sympathetic activation and parasympathetic recovery, maintaining the physiological coherence that every system from immune function to prefrontal cortex performance depends on.
Low HRV means something different and more consequential: the autonomic nervous system is locked in chronic sympathetic dominance — the fight-or-flight state that served survival in acute threat environments but becomes progressively damaging when maintained chronically through the psychological stressors, sleep deprivation, poor nutrition, and sedentary patterns of modern life. Chronic sympathetic dominance is not merely unpleasant. It directly impairs working memory, executive function, and emotional regulation through the prefrontal cortex suppression that sustained stress produces; increases the neuroinflammatory cytokine burden that impairs synaptic plasticity; reduces hippocampal neurogenesis through the cortisol pathway described throughout the Brain Health hub; and increases the long-term risk of cardiovascular disease, immune dysfunction, and metabolic disorder. The HRV number on a tracking device is not merely a fitness metric — it is a real-time readout of the physiological state that determines cognitive performance, stress resilience, and long-term health simultaneously.
HRV training — the deliberate practice of interventions that improve resting HRV over time — is the most targeted available approach to optimizing the autonomic nervous system as a performance substrate. As a certified mindfulness coach with 18+ years of autonomic self-regulation practice, HRV biofeedback has become the measurement tool that quantifies what contemplative practice produces — providing the objective confirmation that allows refinement of the practices that move the metric most effectively. This guide covers the complete science of HRV and autonomic performance, the biofeedback training protocol, and the integrated daily practices that produce meaningful resting HRV improvements across weeks and months.
Part 1: The Science of HRV — What the Number Actually Measures
The Autonomic Nervous System: The Performance Substrate
The autonomic nervous system governs the involuntary physiological processes — heart rate, respiration, digestion, immune function, vascular tone — through its two primary divisions: the sympathetic nervous system (SNS), which activates these systems for energy expenditure and threat response, and the parasympathetic nervous system (PNS), which promotes recovery, repair, digestion, and the physiological restoration that performance requires. Optimal function requires not maximal activation of either division but rapid, efficient switching between them — what is termed autonomic flexibility.
HRV directly reflects this autonomic flexibility. When parasympathetic tone is high, vagal nerve impulses from the brainstem slow the heart rate and produce the high beat-to-beat variability that characterizes a well-regulated, parasympathetically dominant resting state. When sympathetic tone is chronically high — from psychological stress, poor sleep, overtraining, inflammation, or chronic illness — vagal influence on the heart is suppressed, beat-to-beat variability decreases, and the rigid, low-variability heart rhythm pattern of sympathetic dominance emerges. HRV is therefore the most direct available biomarker of vagal tone — which is itself the most accessible indicator of parasympathetic nervous system health.
HRV and Cognitive Performance: The Prefrontal-Vagal Connection
The connection between HRV and cognitive performance is not correlational coincidence — it is anatomically grounded in the prefrontal-vagal pathway that links the brain’s executive control system to cardiac autonomic regulation. Research by Lehrer and Gevirtz established the neurovisceral integration model: the same prefrontal cortex circuits that govern executive function, working memory, attention, and emotional regulation also provide top-down modulation of vagal cardiac control. High vagal tone — reflected in high HRV — indicates that the prefrontal-vagal circuit is intact, well-developed, and actively modulating both cognitive and cardiac function. Low vagal tone indicates impairment of this circuit — with consequences for executive function, attentional control, and emotional regulation that mirror what prefrontal cortex lesion studies produce.
Meta-analytic research by Thayer and colleagues synthesizing 151 studies found that resting HRV is significantly positively correlated with executive function performance across populations — with the relationship holding across attention, working memory, inhibitory control, and cognitive flexibility domains. Individuals with higher resting HRV consistently outperform matched controls on executive function tasks — and HRV biofeedback training that improves HRV produces corresponding improvements in the same executive function domains. This is not a peripheral health metric with incidental cognitive correlates — it is a direct measure of the neural infrastructure that cognitive performance depends on.
What Reduces HRV: The Enemies of Autonomic Flexibility
Understanding HRV suppressors is as actionable as understanding HRV promoters — because the most common features of modern daily life are potent autonomic disruptors. Chronic psychological stress maintains SNS activation and suppresses vagal tone continuously. Sleep deprivation reduces HRV more dramatically than almost any other acute intervention — a single night of poor sleep is reliably detectable in morning HRV readings. Alcohol, even in moderate quantities, significantly suppresses nocturnal HRV through its effects on sleep architecture. Overtraining — accumulated exercise load without adequate recovery — produces declining HRV through unresolved sympathetic stress. Chronic neuroinflammation, poor glycemic control, and sedentary behavior each independently reduce resting HRV through metabolic and inflammatory pathways.
The HRV suppressors list maps almost exactly onto the interventions that the rest of NeuroEdge Formula addresses — confirming that the lifestyle optimization framework across this site is simultaneously an HRV optimization framework. Sleep, anti-inflammatory nutrition, stress management, exercise with adequate recovery, and the reduction of the chronic stressors that maintain sympathetic dominance are the preconditions for HRV training to produce its full effects.
Part 2: HRV Biofeedback Training — The Protocol
Resonance Frequency Breathing: The Core Intervention
Resonance frequency breathing is the most evidence-supported HRV biofeedback technique — and the mechanism that makes it work is elegantly precise. The cardiovascular system has a natural resonance frequency at which heart rate oscillations driven by breathing (respiratory sinus arrhythmia) are maximally amplified through baroreflex feedback — producing the largest possible HRV oscillations and the strongest baroreflex training stimulus. For most adults, this resonance frequency is approximately 6 breaths per minute (0.1 Hz) — though it varies between 4.5 and 7 breaths per minute between individuals.
When breathing is paced at the individual resonance frequency, each breath cycle produces a complete acceleration-deceleration cycle in heart rate, with the oscillation amplitude maximized by the constructive interference between the respiratory and baroreflex feedback systems. The baroreflex — the baroreceptor feedback loop that buffers blood pressure fluctuations — is trained by each cycle of resonance frequency breathing, progressively increasing baroreflex sensitivity and vagal gain. Research by Lehrer and colleagues found that 10 weeks of daily HRV biofeedback training produced significant increases in resting HRV, baroreflex sensitivity, and asthma symptom control — with the training effects persisting for months after the formal training period ended.
Finding individual resonance frequency: The standard starting point is 6 breaths per minute — 5-second inhale, 5-second exhale. Using an HRV biofeedback device or app while breathing at this rate, observe whether the HRV oscillation amplitude is maximized. If the HRV graph shows larger oscillations at 5.5 or 6.5 breaths per minute, adjust accordingly. Most people find their resonance frequency within 0.5 breaths per minute of 6, making this adjustment a refinement rather than a major search.
The 20-Minute Daily Training Protocol
Setup: A quiet environment with minimal distractions. An HRV biofeedback device — consumer options including the Polar H10 chest strap with the Elite HRV app, or the Inner Balance sensor, provide sufficient accuracy for training purposes. Seated or supine position — lying down produces slightly higher HRV readings but may promote drowsiness in some people.
Session structure: 2-minute baseline HRV measurement at normal breathing. 15-minute resonance frequency breathing at the paced rate — 5-second inhale through the nose, 5-second exhale through the nose or mouth. Focus on the breath rhythm rather than monitoring the HRV graph during the session — attentional engagement with the breathing itself improves the coherence response. 3-minute return to normal breathing with a final HRV measurement for session comparison.
Frequency: Daily practice produces the most consistent HRV improvement — research supports that 20 minutes per day produces meaningful resting HRV increases within 4–6 weeks. Twice-daily sessions accelerate improvement when motivation and schedule allow. Minimum effective dose is approximately 20 minutes 5 days per week — below this frequency, the baroreflex training stimulus is insufficient for consistent resting HRV elevation.
Progression: As resting HRV improves over weeks, the resonance frequency breathing produces increasingly large oscillation amplitudes — a positive feedback that confirms the baroreflex sensitivity gains the training is producing. Many practitioners additionally find that resonance frequency breathing becomes a reliable acute stress regulation tool — producing rapid HRV elevation and sympathetic downregulation within 2–3 minutes that provides an immediate cognitive performance reset during high-demand work periods.
Free Download
Get the 7-Day Brain Optimization Protocol
The evidence-based diet, sleep, and supplement framework for your first week of cognitive enhancement — completely free.
Join 2,000+ readers optimizing their cognitive performance. Unsubscribe anytime.
Part 3: Complementary HRV-Elevating Practices
Resonance frequency breathing is the most targeted HRV biofeedback intervention — but several complementary practices produce HRV improvements through independent mechanisms that compound with the biofeedback training rather than duplicating it.
Mindfulness Meditation: Attentional Training and Vagal Development
Mindfulness practice produces HRV improvements through both the sustained attentional training that strengthens prefrontal-vagal connectivity and the reduction of rumination-driven sympathetic activation that chronic psychological stress maintains. Research by Hölzel and colleagues on 8-week mindfulness programs found not only the structural brain changes described in the neuroplasticity guide but also significant HRV improvements — reflecting the autonomic normalization that reduced stress reactivity and improved parasympathetic tone produce. As a certified mindfulness coach, I have consistently observed that practitioners who combine formal mindfulness with resonance frequency breathing show faster and more sustained HRV improvement than those who practice either alone — the mindfulness practice reduces the psychological stressor burden that limits how high HRV can rise, while the biofeedback training directly trains the baroreflex that determines the physiological ceiling.
Protocol: 15–20 minutes daily mindfulness in the morning, combined with 20 minutes resonance frequency breathing — either sequential or at separate times of day. Both practices reinforce the same prefrontal-vagal network from different angles: mindfulness through top-down attentional training, resonance frequency breathing through bottom-up baroreflex conditioning.
Aerobic Exercise: The BDNF-HRV Connection
Regular aerobic exercise improves resting HRV through multiple mechanisms: reduced resting heart rate (directly increasing the absolute HRV available at any given average heart rate), improved baroreflex sensitivity from cardiovascular fitness training, reduced neuroinflammatory burden, and better sleep quality that restores nocturnal HRV. The exercise-HRV relationship is dose-dependent and consistent across populations — with 150+ minutes per week of moderate aerobic exercise producing meaningful resting HRV improvements within 8–12 weeks of consistent practice. The combination of regular aerobic exercise with resonance frequency breathing training produces HRV improvements substantially faster than either alone — with research suggesting the combination may reach HRV levels in 8 weeks that exercise alone achieves in 16.
Cold Exposure: Autonomic Flexibility Training Through Thermal Stress
As established in the cold exposure guide, regular cold exposure produces autonomic adaptation that improves HRV through enhanced sympathetic-parasympathetic switching efficiency. The acute sympathetic activation of cold exposure followed by the recovery period is essentially involuntary autonomic flexibility training — repeatedly exercising the transition between sympathetic activation and parasympathetic recovery in a way that progressively increases the speed and completeness of both transitions. Cold exposure and resonance frequency breathing both improve HRV but through complementary mechanisms — cold exposure trains sympathetic activation and recovery, while resonance frequency breathing trains parasympathetic dominance and baroreflex sensitivity — making their combination more comprehensive than either alone.
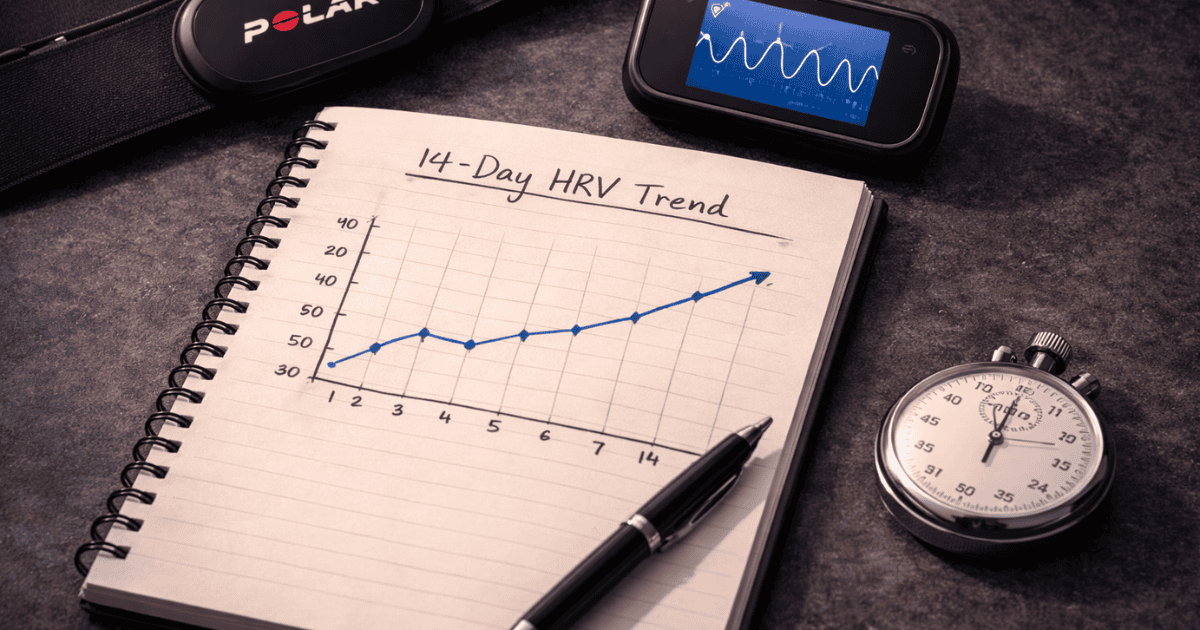
Using HRV as a Daily Performance Guide
Beyond its role as a training target, resting morning HRV provides the most actionable daily readout of physiological recovery status available from consumer devices. The practical application: measure resting HRV within the first 5 minutes of waking (before rising, to avoid posture effects), using a consistent protocol — same device, same position, same duration. Track the rolling average HRV over 7–14 days as the individual baseline. When morning HRV is meaningfully below baseline (typically 10–15% or more), this signals incomplete physiological recovery — warranting reduced training intensity, increased recovery focus, and investigation of the acute stressor (poor sleep, illness onset, accumulated stress) driving the suppression.
The cognitive performance implication is direct: low HRV mornings typically predict reduced executive function, working memory, and stress resilience for the day — making them the appropriate times to reduce cognitive demands, front-load routine tasks, and delay high-stakes decision making to higher-HRV days when the prefrontal-vagal infrastructure is more fully online. Used this way, HRV becomes not merely a training metric but a decision-support tool that allows proactive performance management rather than reactive discovery of impairment after it has already affected outcomes.
Frequently Asked Questions About HRV Training
What is HRV and why does it matter for cognitive performance?
Heart rate variability (HRV) is the variation in time between consecutive heartbeats — measured in milliseconds. A high HRV does not mean irregular heart rhythm; it means the autonomic nervous system is flexibly modulating heart rate in response to breathing, activity, and physiological demands — reflecting healthy parasympathetic nervous system tone and autonomic flexibility. HRV matters for cognitive performance because of the prefrontal-vagal connection: the same prefrontal cortex circuits that govern working memory, attention, inhibitory control, and emotional regulation also provide top-down modulation of cardiac vagal control. High vagal tone — reflected in high HRV — indicates that this prefrontal-vagal circuit is functioning well, with consequences for cognitive performance that Thayer’s meta-analysis of 151 studies confirmed: resting HRV is significantly positively correlated with executive function across all domains measured. Low HRV indicates chronic sympathetic dominance — the physiological state associated with impaired prefrontal function, reduced working memory capacity, worse emotional regulation, and diminished stress resilience. Daily resting HRV measurement therefore provides the most accessible real-time readout of the physiological infrastructure that cognitive performance depends on — and HRV biofeedback training that improves resting HRV produces corresponding improvements in the executive function domains that the biofeedback addresses.
How do I increase HRV naturally?
HRV can be meaningfully increased through several complementary approaches that address different components of the autonomic regulation system. The most targeted intervention is resonance frequency breathing — slow diaphragmatic breathing at approximately 6 breaths per minute (5-second inhale, 5-second exhale) for 20 minutes daily, which directly trains baroreflex sensitivity and vagal gain through the constructive interference of respiratory and cardiac oscillations at the cardiovascular system’s natural resonance frequency. Regular aerobic exercise (150+ minutes per week) improves resting HRV through reduced resting heart rate, improved baroreflex sensitivity, and better sleep quality. Sleep optimization is the highest-leverage single HRV intervention available — consistently inadequate or poor-quality sleep suppresses HRV more dramatically than almost any other factor, and sleep improvements produce immediate HRV gains. Mindfulness meditation improves HRV through reduced rumination-driven sympathetic activation and strengthened prefrontal-vagal connectivity. Cold exposure improves autonomic flexibility through the sympathetic-parasympathetic switching training of repeated thermal stress adaptation. Alcohol reduction produces rapid HRV improvement — even moderate alcohol consumption significantly suppresses nocturnal HRV, and elimination produces measurable improvements within days. Anti-inflammatory dietary changes reduce the cytokine-driven HRV suppression of chronic neuroinflammation. The most impactful single change for most people is sleep — improve sleep quality and duration consistently, and HRV improvement follows almost immediately. The biofeedback training then amplifies what the lifestyle foundation makes possible.
What is a good HRV score?
HRV scores are highly individual and age-dependent — making population norms less useful than individual trend tracking for most practical purposes. That said, some general reference ranges help contextualize where a given measurement sits. The most commonly reported HRV metric from consumer devices (RMSSD — root mean square of successive differences) shows wide population variation: in the 20–25 age range, population averages are typically 55–70ms; in the 30–35 range, 45–60ms; in the 40–45 range, 35–50ms; in the 50–55 range, 25–45ms; in the 60+ range, 20–35ms. Fit, healthy individuals with regular aerobic exercise, good sleep, and low stress typically sit in the upper quartile of their age range. Elite endurance athletes often show RMSSD values 50–100% above age-population averages. The more practically useful metric than absolute score is trend relative to personal baseline: an individual whose resting HRV is consistently 15% below their 14-day average is experiencing meaningful physiological stress regardless of whether the absolute number is 25ms or 75ms. HRV biofeedback training typically produces RMSSD improvements of 10–30% over 8–12 weeks of consistent practice — measurable and clinically meaningful improvements that reflect the genuine autonomic function improvements the training produces rather than device artifact.
How long does it take for HRV biofeedback to work?
HRV biofeedback produces changes across two distinct timescales: acute within-session effects and long-term resting HRV improvements. Within a single resonance frequency breathing session, HRV coherence (the amplitude and regularity of heart rate oscillations at the resonance frequency) increases significantly within the first 3–5 minutes of paced breathing — reflecting the immediate baroreflex response to resonance frequency stimulation. This acute coherence increase is accompanied by real-time improvements in subjective calm and cognitive clarity that many practitioners use as an on-demand stress regulation tool. Long-term resting HRV improvements — the structural autonomic changes reflecting improved vagal tone and baroreflex sensitivity — develop over 4–12 weeks of consistent daily practice. Research by Lehrer and colleagues found significant resting HRV and baroreflex sensitivity improvements after 10 weeks of daily practice, with effects persisting for months after formal training ended. The practical timeline: most practitioners notice improved acute stress regulation within the first 2 weeks; meaningful resting HRV improvement (5–15% above pre-training baseline) typically emerges at weeks 4–6; maximum improvement from a consistent training period is typically reached at weeks 10–16. The training effects are retained for months with reduced maintenance practice — unlike many performance interventions that require continuous full protocol application to maintain gains.
HRV Training: The Measurable Path to Autonomic Performance
HRV training occupies a unique position in the NeuroEdge Formula protocol: it is simultaneously a measurement system, a training intervention, and a daily decision-support tool. It provides the objective quantification that makes the autonomic nervous system — previously invisible and largely unmanageable — legible and trainable. The resting HRV trend over weeks of consistent biofeedback training, sleep optimization, mindfulness practice, and cold exposure is the most comprehensive available confirmation that the stress resilience and cognitive performance infrastructure is improving — not merely the subjective impression of improvement, but the measurable physiological substrate of it.
The integration with the full NeuroEdge Formula protocol is synergistic in every direction: the sleep optimization from the Sleep hub directly improves HRV by restoring nocturnal parasympathetic recovery; the mindfulness practice strengthens the prefrontal-vagal connectivity that HRV reflects; the cold exposure trains the autonomic flexibility that HRV measures; the anti-inflammatory nutrition removes the cytokine burden that suppresses HRV; and the aerobic exercise produces the cardiovascular fitness improvements that increase resting HRV across the broader autonomic system. HRV biofeedback training is the targeted intervention that maximizes these gains — the direct training of the baroreflex that translates lifestyle optimization into the measurable autonomic improvement that the HRV number confirms.
For the complete biohacking context, see the biohacking pillar guide. For the cold exposure protocols that compound with HRV training for autonomic optimization, see the cold exposure guide. For the mindfulness practice that addresses the psychological stressor burden limiting HRV improvement, see the mindfulness section of the brain health guide. The final article in this hub — Advanced Nootropic Stacking Protocols — follows next.
References
- Lehrer, P.M., & Gevirtz, R. (2014). Heart rate variability biofeedback: How and why does it work? Frontiers in Psychology, 5, 756. PubMed
- Thayer, J.F., et al. (2012). A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neuroscience & Biobehavioral Reviews, 36(2), 747–756. PubMed
- Lehrer, P., et al. (2004). Heart rate variability biofeedback increases baroreflex gain and peak expiratory flow. Psychosomatic Medicine, 66(5), 796–805. PubMed
- Hölzel, B.K., et al. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging, 191(1), 36–43. PubMed
- Mäkinen, T.M., et al. (2008). Autonomic nervous function during whole-body cold exposure before and after cold acclimation. Journal of Applied Physiology, 105(5), 1523–1531. PubMed
- Shaffer, F., & Ginsberg, J.P. (2017). An overview of heart rate variability metrics and norms. Frontiers in Public Health, 5, 258. PubMed
- Pagani, M., et al. (1997). Power spectral analysis of heart rate and arterial pressure variabilities as a marker of sympatho-vagal interaction in man and conscious dog. Circulation Research, 59(2), 178–193. PubMed
- Task Force of the European Society of Cardiology. (1996). Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Circulation, 93(5), 1043–1065. PubMed
- Zaccaro, A., et al. (2018). How breath-control can change your life: A systematic review on psycho-physiological correlates of slow breathing. Frontiers in Human Neuroscience, 12, 353. PubMed
- Vaschillo, E.G., et al. (2006). Characteristics of resonance in heart rate variability stimulated by biofeedback. Applied Psychophysiology and Biofeedback, 31(2), 129–142. PubMed
Tags: HRV training stress optimization, heart rate variability cognitive performance, HRV biofeedback, resonance frequency breathing, vagal tone cognitive performance, HRV and executive function, how to increase HRV, HRV biofeedback protocol, baroreflex sensitivity training, autonomic nervous system performance, HRV stress resilience, prefrontal vagal connection, resting HRV improvement, HRV mindfulness, HRV cold exposure
About Peter Benson
Peter Benson is a cognitive enhancement researcher and certified mindfulness coach with 18+ years of autonomic self-regulation practice and expertise in HRV-guided performance optimization. He uses HRV biofeedback as both a training tool and a daily performance readout, integrating it with mindfulness practice, cold exposure, and the complete NeuroEdge Formula protocol. NeuroEdge Formula is his platform for sharing rigorous, safety-first cognitive enhancement guidance.