The Complete Guide to Better Sleep: Evidence-Based Strategies for Deep, Restorative Rest
Medical Disclaimer: The information in this article is for educational purposes only and does not constitute medical advice. If you are experiencing significant sleep difficulties, consult a qualified healthcare provider. Sleep disorders including sleep apnea, insomnia disorder, and circadian rhythm disorders require professional evaluation. Always consult a healthcare provider before beginning any supplement regimen. Individual responses vary.
Sleep is the most powerful cognitive enhancement intervention available — and the most neglected. It is free, requires no supplements, and produces benefits across every dimension of cognitive and physical performance that no drug, protocol, or optimization strategy can match when it is absent. Yet most people approach sleep as the passive default state of an exhausted body rather than the active, precisely orchestrated neurobiological process it actually is — a process that can be deliberately optimized with the same precision applied to diet, training, or supplementation.
After 18+ years researching cognitive enhancement, I have reached one consistent conclusion: no nootropic stack, no morning protocol, no focus strategy produces its intended effect on top of chronic sleep deprivation. Sleep is not one pillar among many — it is the foundation that every other optimization effort stands on. Optimize it first, optimize everything else on top of it, and the compound effect is extraordinary. Neglect it while optimizing everything else, and you are building on sand.
This is the complete, evidence-based guide to better sleep — covering the neuroscience of sleep architecture, the specific behavioral strategies with the strongest research support for improving sleep quality and duration, the supplementation compounds that directly support the neurobiological mechanisms of deep sleep, and the common mistakes that undermine sleep quality in ways most people never identify. It is the pillar guide for the Sleep hub, connecting to the detailed guides on sleep and memory consolidation, sleep architecture, falling asleep faster, and the supplement guides for the compounds that most directly support sleep quality.
Part 1: What Sleep Actually Is — The Neuroscience
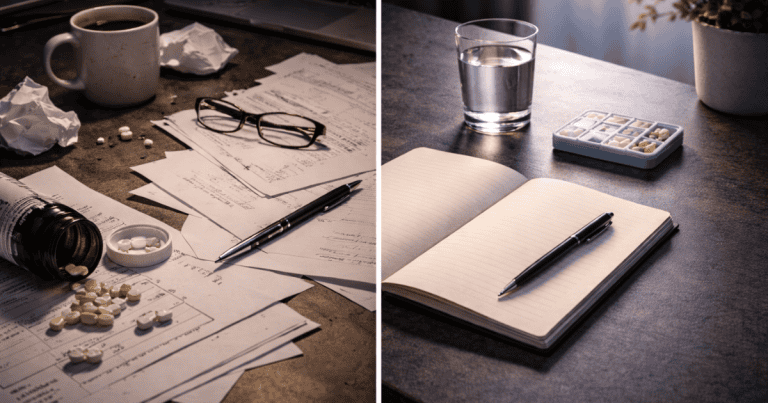
Sleep is not unconsciousness. It is a precisely regulated sequence of neurological states — each with distinct brain activity patterns, neurotransmitter profiles, and biological functions — that the brain cycles through in a predictable architecture across the night. Understanding this architecture is what makes sleep optimization possible, because different aspects of sleep quality correspond to different stages, and the interventions that improve one stage can differ entirely from those that improve another.
Sleep Architecture: The Four Stages
A complete sleep cycle lasts approximately 90 minutes and consists of four stages that repeat 4–6 times across a full night. The proportion of each stage within cycles changes across the night in ways that have direct implications for optimization.
NREM Stage 1 (N1) is the light sleep transition — the hypnagogic state between wakefulness and sleep lasting 1–7 minutes. Brain activity shifts from alpha waves (relaxed wakefulness) to theta waves (light sleep), and the person remains easily awakened. N1 is neurologically necessary as the entry point to deeper sleep but produces no significant restorative benefit on its own.
NREM Stage 2 (N2) is consolidated light sleep — lasting approximately 20 minutes per cycle and accounting for roughly 50% of total sleep time across the night. N2 is characterized by sleep spindles (bursts of 12–15 Hz thalamo-cortical activity) and K-complexes (large-amplitude slow waves that suppress external arousal). Sleep spindles during N2 are the same mechanism responsible for memory consolidation discussed in the sleep and memory guide — making N2 sleep quality a direct memory performance variable.
NREM Stage 3 (N3) — Slow Wave Sleep is the deepest and most physically and cognitively restorative sleep stage. Research on slow wave sleep and restoration established that SWS is the primary stage for physical restoration (growth hormone release, tissue repair, immune function), declarative memory consolidation, and metabolic waste clearance from the brain through the glymphatic system. SWS is concentrated in the first half of the night and is the stage most severely reduced by alcohol, sleep debt, aging, and poor sleep hygiene. Optimizing SWS depth and duration is the highest-value sleep quality target.
REM Sleep — the stage of vivid dreaming — is characterized by near-complete muscle atonia, rapid eye movements, and brain activity that closely resembles wakefulness. REM sleep is concentrated in the second half of the night and is responsible for emotional memory processing, creative integration of new information with existing knowledge, procedural memory consolidation, and the regulation of emotional reactivity. REM is the stage most severely truncated by short sleep — the final sleep cycles that contain the most REM are the first to be lost when sleep is shortened.
The Glymphatic System: Sleep as Brain Detoxification
One of the most significant recent discoveries in sleep neuroscience is the glymphatic system — the brain’s waste clearance mechanism that operates almost exclusively during sleep. Research by Xie and colleagues found that during sleep — particularly SWS — cerebrospinal fluid flows through channels surrounding brain blood vessels, flushing out metabolic waste products including amyloid-beta and tau proteins — the same proteins that accumulate in Alzheimer’s disease when glymphatic clearance is chronically impaired. The glymphatic system is approximately 10 times more active during sleep than during wakefulness, and its function is directly dependent on sleep depth — making SWS optimization simultaneously a cognitive performance strategy and a long-term brain health intervention.
Why You Feel Sleepy: Adenosine and the Circadian Clock
Sleepiness is governed by two independent biological systems operating simultaneously. The first is adenosine — a metabolic byproduct of neural activity that accumulates in the brain throughout wakefulness, progressively increasing sleep pressure. Every hour awake produces more adenosine; sleep clears it. Caffeine works by blocking adenosine receptors — delaying the subjective experience of sleepiness without reducing actual adenosine accumulation. When caffeine wears off, the accumulated adenosine floods unblocked receptors simultaneously — the “caffeine crash.”
The second system is the circadian clock — the suprachiasmatic nucleus (SCN) in the hypothalamus that generates a ~24-hour oscillation in alertness, independently of adenosine accumulation. The circadian clock determines not just when you feel sleepy but the timing, depth, and composition of sleep stages throughout the night. It is primarily entrained by light — morning light exposure advances the circadian phase (making sleep and wake times earlier) while evening light exposure delays it (pushing sleep and wake times later). Consistent circadian entrainment is the single most impactful structural intervention for sleep quality — it determines the neurochemical conditions under which every other sleep optimization strategy operates.
Part 2: The Evidence-Based Behavioral Strategies for Better Sleep
The behavioral strategies with the strongest evidence for sleep improvement address the two biological systems governing sleep: circadian entrainment (timing) and adenosine/homeostatic sleep pressure (depth). Applied consistently, they produce more reliable sleep improvement than any supplement — and provide the biological foundation on which supplementation produces its maximum effect.
Consistent Sleep and Wake Timing: The Non-Negotiable Foundation
The single most impactful sleep quality intervention available is consistent sleep and wake timing — the same bedtime and wake time within a 30-minute window every day including weekends. Research on social jetlag found that circadian misalignment from inconsistent sleep timing — the common pattern of sleeping later and waking later on weekends than weekdays — produces measurable cognitive impairments, metabolic disruptions, and sleep quality reductions independent of total sleep duration. The circadian clock builds expectation of sleep and wake times through consistent entrainment — and inconsistency prevents the deep SWS and REM cycling that consistent timing enables.
The practical protocol: choose a wake time that allows 7–9 hours of sleep before it and maintain it every day — including weekends, regardless of when you fell asleep. The wake time anchors the circadian clock; the bedtime becomes self-regulating as sleep pressure and circadian alignment converge at the appropriate hour. This is uncomfortable initially for weekend night owls, but the circadian quality dividend within 2–3 weeks of consistency is the most significant sleep improvement most people experience from any single behavioral change.
Morning Light Exposure: Anchoring the Circadian Clock
Bright light exposure within 30–60 minutes of waking is the most powerful circadian entrainment signal available — directly advancing the circadian clock and anchoring it to a consistent phase. Research on morning light and circadian entrainment found that outdoor light exposure (even on cloudy days, outdoor light is 10–50x brighter than typical indoor lighting) within the first hour of waking significantly reduces sleep onset latency at the subsequent night’s bedtime and increases SWS depth — because a well-anchored circadian clock generates more robust melatonin onset at the appropriate evening time.
Ten to twenty minutes of outdoor light exposure — walking, sitting outside, morning exercise outdoors — within 60 minutes of waking is the complete protocol. On overcast days, the duration can extend to 20–30 minutes to compensate for reduced light intensity. This single habit, applied consistently, produces measurable improvements in sleep onset and sleep depth within 1–2 weeks — and its effects compound with consistent wake timing to produce the most powerful non-pharmacological sleep entrainment protocol available.
Temperature Optimization: The Thermal Gateway to Deep Sleep
Core body temperature must drop by approximately 1–2°C to initiate and maintain deep SWS — and the bedroom environment is the primary determinant of how efficiently this thermoregulatory drop occurs. Research on bedroom temperature and sleep architecture found that room temperatures between 65–68°F (18–20°C) optimize the thermal gradient required for deep SWS, while temperatures above 70°F consistently reduce SWS depth and REM duration even when total sleep time is maintained.
A warm shower or bath 60–90 minutes before bed accelerates core temperature drop through peripheral vasodilation — the body responds to the surface warming by radiating heat outward, lowering core temperature more rapidly than it would through passive cooling alone. This bath-induced temperature drop produces measurably faster sleep onset and deeper SWS in the subsequent sleep period — a counterintuitive but well-replicated finding that makes the pre-bed warm shower one of the most evidence-supported behavioral sleep interventions available.
Light Elimination: Protecting Melatonin Production
Any light during sleep — including low-level light from electronics, street lighting through curtains, or LED standby indicators — activates retinal photoreceptors that signal the SCN to suppress melatonin production. Even dim light (as low as 10 lux — the brightness of a typical room with lights dimmed) produces measurable melatonin suppression and reduces SWS depth.
Complete light elimination through blackout curtains or a sleep mask is the simplest and most cost-effective SWS quality intervention available. In the 2–3 hours before bed, avoiding bright overhead lights and shifting to dim, warm-toned lighting (or blue-light-blocking glasses) protects the natural melatonin rise that initiates sleep onset — allowing sleep to begin at the circadian-appropriate time rather than artificially delayed by artificial light exposure.
Caffeine Timing: The 10-Hour Rule
Caffeine’s adenosine-blocking mechanism impairs sleep quality in ways that extend far beyond subjective sleepiness. Research on caffeine and sleep architecture found that caffeine consumed even 6 hours before bed reduces SWS by a measurable amount — with effects persisting because caffeine’s half-life is 5–7 hours and its quarter-life (25% of peak blood concentration) is 10–14 hours. An afternoon coffee at 2pm still has 25% of its adenosine-blocking effect at midnight for many individuals.
The evidence-based protocol: last caffeine intake by noon for individuals with average caffeine metabolism (half-life of 5–6 hours). For individuals who metabolize caffeine slowly — often identifiable by sensitivity to afternoon coffee disrupting sleep even hours later — cutting off by 10am produces better results. The 60–90 minute caffeine delay from waking (described in the morning routine guide) combined with the noon cutoff produces the cleanest adenosine dynamics across the full day.
Alcohol: The Sleep Quality Destroyer
Alcohol is one of the most aggressively marketed sleep aids and one of the most damaging to actual sleep quality. While alcohol accelerates sleep onset through GABAergic sedation, it produces compensatory neurological activation in the second half of the night — fragmenting sleep, suppressing REM, and reducing SWS depth. Research on alcohol and sleep architecture found dose-dependent reductions in REM sleep and increased sleep fragmentation across the full night — even when alcohol has been fully metabolized — because the neurological rebound from the initial GABAergic suppression persists through the night. Any alcohol within 4 hours of bed meaningfully impairs sleep quality; the common belief that a drink helps you sleep better is the sedation-sleep confusion — falling asleep faster while sleeping less deeply and less restoratively.
Free Download
Get the 7-Day Brain Optimization Protocol
The evidence-based diet, sleep, and supplement framework for your first week of cognitive enhancement — completely free.
Join 2,000+ readers optimizing their cognitive performance. Unsubscribe anytime.
Part 3: The Evidence-Based Supplementation Stack for Better Sleep
The behavioral strategies above address the circadian and homeostatic systems that govern sleep architecture. The supplementation layer optimizes the neurochemical conditions within that architecture — directly supporting SWS depth, melatonin production, and the stress management that is the most common biological obstacle to quality sleep.
Magnesium L-Threonate — SWS Depth and Sleep Spindle Enhancement
Magnesium L-Threonate is the highest-priority sleep supplement in the NeuroEdge stack — not merely because of its direct sleep quality benefits but because of the convergence of its sleep and cognitive effects. MgT’s GABAergic and NMDA receptor modulatory effects directly support the neurological conditions for SWS induction and sleep spindle generation, while its synaptic density benefits and cognitive improvements operate through the same night’s sleep that the supplementation improves. At 1,500–2,000mg daily (divided doses, with the larger portion taken 1–2 hours before bed), MgT consistently improves sleep onset, sleep efficiency, and subjective sleep quality — while simultaneously optimizing the memory consolidation that occurs during the sleep it improves.
Ashwagandha KSM-66 — Cortisol Management and Sleep Initiation
Elevated evening cortisol is the most common biological cause of delayed sleep onset and reduced SWS depth in cognitively active adults — and Ashwagandha KSM-66 is the most evidence-supported botanical for cortisol reduction. Research on Ashwagandha and sleep quality found significant improvements in sleep onset latency, total sleep time, sleep efficiency, and morning alertness after 8 weeks of supplementation in individuals with self-reported sleep problems — with the mechanism clearly linked to HPA axis modulation and cortisol reduction. At 300–600mg of KSM-66 extract taken in the evening, Ashwagandha addresses the stress-driven sleep disruption that behavioral sleep hygiene alone cannot resolve when the underlying cortisol elevation remains unaddressed.
L-Theanine — Relaxed Alpha-Wave State for Sleep Transition
L-theanine at 200–400mg taken 30–60 minutes before bed promotes the alpha-wave brain state — relaxed alertness without sedation — that facilitates the transition from wakefulness to sleep without producing the next-day grogginess associated with sedative compounds. Research on L-theanine and sleep quality found improvements in sleep efficiency and reduced sleep fragmentation, with the mechanism involving enhanced GABAergic activity and the alpha-wave promotion that reduces the cognitive hyperarousal — racing thoughts, mental rehearsal of the day’s events — that is the most common subjective obstacle to sleep onset. L-theanine is non-sedating and non-habit-forming, making it appropriate for nightly use without tolerance development.
What About Melatonin?
Melatonin is the most widely used sleep supplement globally — and also the most commonly misused. Melatonin is a circadian timing signal, not a sedative or sleep-depth enhancer. It signals the brain that it is biologically nighttime — shifting the circadian phase — but does not directly increase SWS depth, REM duration, or sleep efficiency beyond their circadian-appropriate levels. The appropriate use cases for melatonin are circadian phase shifting: jet lag recovery, shift work adaptation, and correcting delayed sleep phase (the night owl pattern of falling asleep very late). For these applications, low-dose melatonin (0.5–1mg) taken at the target bedtime is effective. For general sleep quality improvement in individuals with normal circadian alignment, melatonin adds little beyond placebo — while the behavioral strategies and MgT/Ashwagandha/L-theanine stack produces the SWS and REM improvements that actual sleep quality depends on.
Part 4: The Complete Sleep Optimization Protocol
The complete sleep optimization protocol integrates behavioral strategies and supplementation into a coherent daily structure — addressing circadian timing, sleep pressure dynamics, temperature, light, and neurochemical conditions simultaneously.
Morning Anchors (7:00am example, adjust to your target wake time)
Wake at consistent time — no snooze. Within 30 minutes: 10–20 minutes of outdoor light exposure (combined with morning walk or exercise for maximum circadian and BDNF benefit). Delay caffeine by 60–90 minutes from waking — allowing the cortisol awakening response to complete before caffeine is introduced. Last caffeine by noon.
Evening Wind-Down (90 minutes before target sleep)
Dim overhead lights — shift to warm, low-level lighting or blue-light-blocking glasses. Warm shower or bath 60–90 minutes before bed for the core temperature-drop effect. Avoid screens with bright backlighting directly before bed; if screen use is unavoidable, blue-light-blocking glasses are the practical mitigation. No alcohol within 4 hours of target sleep time.
Supplementation timing: MgT 500–1,000mg (evening portion) + Ashwagandha 300–600mg + L-theanine 200–400mg — all taken 60–90 minutes before bed.
Pre-Sleep Transition (30 minutes before bed)
Brief active recall review of the day’s most important learning — 10 minutes maximum, reconstructing key concepts from memory. This seeds the hippocampal consolidation queue for the night’s SWS replay cycles without producing the cognitive activation that extended evening study creates. Then deliberate cognitive wind-down: reading physical books, light journaling to close mental open loops, breathing exercises. Bedroom completely dark and at 65–68°F.
Common Sleep Mistakes That Undermine Everything Else
Lying in bed awake: Extended wakefulness in bed trains the brain to associate the bed with wakefulness rather than sleep — the mechanism of learned insomnia. If you have not fallen asleep within 20 minutes, leave the bedroom and engage in quiet, non-stimulating activity until sleepy, then return. This stimulus control principle is the most evidence-supported behavioral intervention for chronic sleep onset difficulty.
Weekend sleep schedule drift: Even a single hour of later waking on weekends shifts the circadian clock in the direction of delayed sleep phase — making Monday night sleep onset difficult and producing the Monday morning grogginess that most people attribute to “hating Mondays” rather than to self-induced social jetlag.
Compensatory napping for chronic sleep debt: Long afternoon naps (90+ minutes) taken to compensate for chronic insufficient nighttime sleep reduce the adenosine accumulation (sleep pressure) that drives deep SWS at the subsequent night’s sleep onset — producing shallower sleep that fails to fully discharge sleep debt and perpetuates the cycle. If napping is necessary, limiting naps to 20 minutes before 2pm preserves nighttime sleep pressure while providing the alertness benefit of the nap.
Exercising too late: Vigorous exercise within 3–4 hours of bed elevates core body temperature and sympathetic nervous system activation in ways that delay sleep onset and reduce initial SWS depth for temperature-sensitive individuals. Morning or early afternoon exercise produces all the sleep-promoting BDNF and adenosine benefits without the temperature conflict.
Frequently Asked Questions About Better Sleep
How many hours of sleep do adults actually need?
Research consistently establishes 7–9 hours as the range within which most adults achieve complete sleep cycling — sufficient SWS for physical restoration and memory consolidation, and sufficient REM for emotional processing and creative integration. Below 7 hours, cognitive impairments accumulate even when subjective sleepiness is absent — research has found that individuals chronically sleeping 6 hours show performance deficits equivalent to going 24 hours without sleep, while rating themselves as only slightly sleepy. The 8-hour recommendation is not arbitrary: it reflects the duration required for 4–5 complete 90-minute sleep cycles, with the SWS-dominant early cycles and REM-dominant late cycles both completing fully. Genetic variants that allow optimal function on less than 7 hours exist but are extremely rare — estimated at less than 3% of the population. For most people claiming to function well on 6 hours, adaptation to chronic sleep deprivation has reduced their perception of impairment without reducing the actual impairment itself.
What is the most effective thing you can do for better sleep tonight?
For immediate improvement tonight, the highest-impact single intervention is temperature — set your bedroom to 65–68°F and take a warm shower 60–90 minutes before your target bedtime. The shower-induced core temperature drop through peripheral vasodilation produces measurably faster sleep onset and deeper SWS in the subsequent sleep period. Eliminate all light sources from the bedroom completely. Take L-theanine 200–400mg 45–60 minutes before bed to reduce the cognitive hyperarousal that delays sleep onset. Avoid alcohol entirely and stop caffeine at noon if you had any after that time. For sustained improvement over weeks, the behavioral foundation is consistent wake timing every day — the same time regardless of when you fell asleep — which anchors the circadian clock and produces compounding sleep quality improvements across 1–3 weeks of consistency.
Why do I wake up at 3am and can’t get back to sleep?
Waking at 3–4am and being unable to return to sleep is one of the most common sleep complaints in cognitively active adults, and it has several common causes with specific solutions. The most frequent cause is elevated cortisol — chronic stress produces dysregulated cortisol patterns that can include premature early-morning cortisol spikes that trigger arousal before the appropriate wake time. Ashwagandha for cortisol management and consistent stress reduction practices address this mechanism. A second common cause is alcohol — even moderate evening alcohol use produces neurological rebound activation in the second half of the night that causes early arousal. A third cause is the body temperature rising prematurely — if the bedroom is too warm, core temperature rises before the appropriate wake time, triggering arousal. Reducing bedroom temperature and ensuring alcohol avoidance are the highest-priority interventions for mid-night waking. If these environmental and behavioral corrections do not resolve the pattern within 2–3 weeks, consultation with a sleep specialist to rule out sleep apnea or other sleep disorders is appropriate.
Does melatonin actually improve sleep quality?
Melatonin is a circadian timing signal rather than a sleep quality enhancer — it shifts the phase of the circadian clock rather than directly increasing SWS depth or REM duration. Research shows melatonin is effective for jet lag (shifting the circadian clock to a new time zone), delayed sleep phase syndrome (advancing the sleep-wake cycle in chronic night owls), and shift work adaptation — all applications where circadian timing correction is the goal. For individuals with normal circadian alignment who simply want deeper, more restorative sleep, melatonin adds little beyond placebo effect. The compounds that directly improve sleep depth — Magnesium L-Threonate for SWS and sleep spindle enhancement, Ashwagandha for cortisol-driven sleep disruption, and L-theanine for sleep onset anxiety — produce more meaningful sleep quality improvements for the majority of users than melatonin. If melatonin is used for appropriate circadian applications, lower doses (0.5–1mg) are more effective than the 5–10mg doses commonly marketed, as higher doses can produce next-day grogginess and may desensitize melatonin receptors with regular use.
How long does it take to improve sleep quality with behavioral changes?
The timeline for sleep quality improvement from behavioral changes varies by intervention. Consistent wake timing produces measurable circadian entrainment improvements within 1–2 weeks — with sleep onset becoming easier and SWS depth increasing as the circadian clock anchors to the consistent schedule. Morning light exposure compounds this effect and shows benefits within the same week when applied consistently. Temperature optimization (bedroom at 65–68°F, warm pre-sleep shower) produces improvements on the first night of application. Caffeine cutoff changes show sleep quality improvements within days as afternoon adenosine dynamics normalize. Alcohol avoidance shows immediate improvements in sleep architecture from the first alcohol-free night. The supplementation layer — MgT for sleep spindles, Ashwagandha for cortisol management — shows initial sleep quality improvements within 1–2 weeks, with full effects developing over 6–8 weeks of consistent use. The complete integrated protocol — behavioral changes plus supplementation — produces its full compound effect at approximately the 4–8 week mark, at which point most individuals report the most significant sustained sleep quality improvement they have experienced.
Sleep as the Foundation of Everything Else
Every protocol on NeuroEdge Formula — every nootropic stack, every focus strategy, every memory optimization system — assumes an adequately sleeping brain. Sleep is not one optimization target among many. It is the biological substrate that every other target depends on. Optimizing it produces benefits across focus, memory, mood, physical performance, immune function, metabolic health, and long-term brain protection simultaneously — and no combination of supplements, strategies, or interventions produces equivalent benefit when sleep is chronically insufficient.
The complete sleep optimization protocol — consistent timing, morning light, temperature management, light elimination, caffeine and alcohol discipline, and the MgT/Ashwagandha/L-theanine stack — is not complex. It is consistent. Applied nightly for 4–8 weeks, it produces a qualitatively different cognitive baseline that makes every other optimization strategy more effective, every learning session more productive, and every difficult cognitive task more accessible.
Start with the two highest-leverage behavioral interventions: consistent wake time every day, and morning light within 60 minutes of waking. Add the temperature protocol and light elimination the same week. Introduce MgT and Ashwagandha in week two. Within a month, the difference is not subtle.
For the detailed sleep and memory consolidation neuroscience, see the sleep and memory guide. For the full supplement details, see the Magnesium L-Threonate guide and Ashwagandha guide in the Nootropics hub. For the morning protocol that begins where the sleep protocol ends, see the morning routine guide.
References
- Stickgold, R. (2005). Sleep-dependent memory consolidation. Nature, 437(7063), 1272–1278. PubMed
- Xie, L., et al. (2013). Sleep drives metabolite clearance from the adult brain. Science, 342(6156), 373–377. PubMed
- Wittmann, M., et al. (2006). Social jetlag: Misalignment of biological and social time. Chronobiology International, 23(1–2), 497–509. PubMed
- Leproult, R., et al. (1997). Sleep loss results in an elevation of cortisol levels the next evening. Sleep, 20(10), 865–870. PubMed
- Okamoto-Mizuno, K., & Mizuno, K. (2012). Effects of thermal environment on sleep and circadian rhythm. Journal of Physiological Anthropology, 31(1), 14. PubMed
- Drake, C., et al. (2013). Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. Journal of Clinical Sleep Medicine, 9(11), 1195–1200. PubMed
- Ebrahim, I.O., et al. (2013). Alcohol and sleep I: Effects on normal sleep. Alcoholism: Clinical and Experimental Research, 37(4), 539–549. PubMed
- Langade, D., et al. (2019). Efficacy and safety of Ashwagandha root extract in insomnia and anxiety. Cureus, 11(9), e5797. PubMed
- Rao, T.P., et al. (2015). In search of a safe natural sleep aid: L-theanine. Journal of the American College of Nutrition, 34(4), 436–447. PubMed
- Slutsky, I., et al. (2010). Enhancement of learning and memory by elevating brain magnesium. Neuron, 65(2), 165–177. PubMed
Tags: how to get better sleep, sleep optimization, sleep neuroscience, sleep architecture stages, slow wave sleep, REM sleep, glymphatic system sleep, circadian rhythm sleep, morning light sleep, bedroom temperature sleep, caffeine sleep, alcohol sleep quality, Magnesium L-Threonate sleep, Ashwagandha sleep, L-theanine sleep
About Peter Benson
Peter Benson is a cognitive enhancement researcher and mindfulness coach with 18+ years of personal and professional experience in nootropics, neuroplasticity, and sleep optimization protocols. He has personally coached hundreds of individuals through integrated cognitive performance programs combining evidence-based sleep strategies with targeted supplementation. NeuroEdge Formula is his platform for sharing rigorous, safety-first cognitive enhancement guidance.