How to Prevent Cognitive Decline: The Evidence-Based Protocol
Medical Disclaimer: The information in this article is for educational purposes only and does not constitute medical advice. Cognitive changes, memory difficulties, and concerns about cognitive decline require evaluation by a qualified healthcare provider. Nothing in this article substitutes for professional medical assessment. Always consult a healthcare provider before beginning any supplement regimen, particularly if you have pre-existing conditions or take medications.
The question of how to prevent cognitive decline is one of the most important questions in contemporary medicine — and one where the gap between what the research shows and what most people actually do is widest. Dementia affects more than 55 million people worldwide, with Alzheimer’s disease accounting for 60–70% of cases. By 2050, that number is projected to nearly triple. And yet the research increasingly shows that Alzheimer’s and most forms of age-related cognitive decline are not the inevitable consequences of aging — they are the consequences of decades of specific, modifiable neurobiological insults applied to a brain that never had the opportunity to defend itself.
The most important finding in the entire field of dementia prevention research is also its most underappreciated: the pathological processes that produce cognitive decline begin 15–20 years before symptoms appear. Amyloid-beta plaques accumulate silently during what feels like normal cognitive function. Hippocampal volume shrinks gradually through the 40s and 50s. Neuroinflammation builds. Cognitive reserve erodes. By the time memory symptoms emerge in the 60s or 70s, the pathological burden is significant — and the leverage for behavioral intervention, though still meaningful, is far less than in the preceding decades when the brain was still largely asymptomatic.
This guide covers what the research actually shows about preventing cognitive decline — organized around the modifiable risk factors that the evidence most consistently identifies, the specific interventions that address each one, and the integrated protocol that applies them as a coherent daily practice. It builds on the brain health pillar guide and neuroplasticity guide, and connects throughout to the protocols and supplementation guidance across NeuroEdge Formula.
Part 1: The Modifiable Risk Factors — What the Evidence Identifies
The Lancet Commission on Dementia Prevention, Intervention, and Care — the most comprehensive evidence synthesis on dementia risk reduction — identified twelve modifiable risk factors that collectively account for approximately 40% of dementia cases worldwide. This is one of the most significant findings in neurology: nearly half of all dementia is potentially preventable through interventions on factors within individual control. Understanding which factors carry the most weight — and why — is what makes prevention a targeted practice rather than generic “live healthily” advice.
Physical Inactivity: The Largest Single Modifiable Risk Factor
Physical inactivity is the single largest modifiable contributor to dementia risk in the Lancet Commission analysis — accounting for an estimated 17.7% of attributable risk in high-income countries. The mechanism is the BDNF-hippocampal neurogenesis axis established in the neuroplasticity guide: aerobic exercise drives hippocampal volume maintenance, synaptic density preservation, cognitive reserve building, and amyloid-beta reduction through mechanisms that no other single lifestyle factor replicates with comparable magnitude.
Erickson’s research demonstrated that older adults who began an aerobic exercise program showed 2% hippocampal volume increases over 12 months — directly reversing the 1–2% annual hippocampal shrinkage of normal aging. Prospective epidemiological research has found that individuals who maintain regular moderate aerobic exercise across midlife show 30–40% lower dementia incidence in later life compared to sedentary peers. For a preventable disease, that is an extraordinary protective effect from an intervention that costs nothing.
Protocol: 150–180 minutes per week of moderate aerobic exercise (65–75% maximum heart rate), distributed across at least 4 sessions. Begin now — the benefit compounds with years of consistency, and the earlier in midlife the habit is established, the greater the lifetime cognitive reserve built.
Chronic Stress and Depression: The HPA-Hippocampal Axis
Chronic psychological stress and depression are both identified as significant dementia risk factors — and both operate through the glucocorticoid toxicity mechanism on hippocampal structure described in detail in the brain health guide. Elevated cortisol from chronic HPA axis activation directly reduces hippocampal dendritic branching, suppresses neurogenesis, impairs BDNF signaling, and over years produces measurable hippocampal volume reduction. Midlife depression — even when episodic rather than chronic — doubles dementia risk in longitudinal studies, with the mechanism likely involving both the direct hippocampal damage of cortisol dysregulation and the reduced neuroplasticity that depression-associated BDNF suppression produces.
The interventions that most effectively reduce chronic stress-driven HPA dysregulation — aerobic exercise, mindfulness practice, Ashwagandha KSM-66, adequate sleep — are therefore simultaneously anti-depressant and neuroprotective interventions. As a certified mindfulness coach, the consistent pattern I observe is that the individuals who establish regular mindfulness practice in their 40s and 50s show the most marked improvements in stress reactivity, sleep quality, and cognitive baseline across subsequent years — precisely because mindfulness practice addresses the cortisol mechanism that is one of the most damaging common drivers of premature cognitive aging.
Protocol: Daily mindfulness practice 15–20 minutes (documented hippocampal gray matter density increases, HPA normalization). Ashwagandha KSM-66 300–600mg if chronic stress is significant. Treat depression actively rather than accepting it as a normal feature of aging — its hippocampal consequences are preventable.
Poor Sleep: The Amyloid Accumulation Highway
Chronic sleep restriction is emerging as one of the most significant and least recognized modifiable dementia risk factors — for the specific reason that the glymphatic amyloid clearance mechanism operates primarily during SWS, making years of poor sleep quality directly equivalent to years of reduced amyloid-beta clearance. Research by Lucey and colleagues found that even a single night of sleep deprivation significantly increased amyloid-beta levels in cerebrospinal fluid — with the accumulation reversing after recovery sleep, but the implication for chronic restriction being clear: years of insufficient SWS accumulates amyloid-beta toward the pathological threshold that triggers the Alzheimer’s cascade.
Epidemiological data is consistent: individuals reporting consistently less than 6 hours of sleep per night show significantly higher dementia risk in longitudinal studies, with a U-shaped relationship where both very short (<6 hours) and very long (>9 hours) sleep duration associate with increased risk. The very long sleep association likely reflects early-stage pathological processes rather than causality. The short sleep association is mechanistically straightforward: insufficient SWS means insufficient glymphatic clearance, which means progressive amyloid-beta accumulation.
Protocol: The complete sleep optimization protocol from the sleep guide, applied as a non-negotiable neuroprotective priority. Magnesium L-Threonate for SWS depth and sleep spindle enhancement. Ashwagandha for cortisol-driven sleep fragmentation. Consistent 7–9 hour sleep duration with consistent timing.
Cardiovascular Risk Factors: Brain Blood Flow and Vascular Dementia
Hypertension, type 2 diabetes, obesity, and high LDL cholesterol — the metabolic syndrome cluster — each independently increase dementia risk through vascular mechanisms: reduced cerebral blood flow, increased cerebrovascular disease burden, blood-brain barrier dysfunction, and neuroinflammation from metabolic dysregulation. The MIND diet research by Morris and colleagues found that dietary patterns optimized for brain health reduced Alzheimer’s risk by 53% — through the combined effects of reducing vascular risk factors, lowering neuroinflammation, and providing the specific nutrients (DHA, polyphenols, B vitamins) that neuronal maintenance requires.
The connection between cardiovascular and brain health is so direct that the phrase “what is good for the heart is good for the brain” is not a metaphor — it is a description of overlapping vascular mechanisms. Managing blood pressure into the normal range, maintaining healthy metabolic function, and avoiding smoking are among the highest-impact single dementia risk reduction interventions available — and they compound with the neuroplasticity-specific interventions rather than competing with them.
Social Isolation and Cognitive Disengagement
Social isolation and low educational or cognitive engagement are both identified as significant dementia risk factors through the cognitive reserve mechanism: the brain that is consistently challenged, engaged, and stimulated across midlife builds the synaptic density and network complexity that buffer against pathological damage. Stern’s research on cognitive reserve found that individuals with higher lifetime cognitive engagement — education, intellectually demanding occupations, continuous learning, social connection — showed significantly delayed symptom onset despite equivalent pathological burden at autopsy, confirming the reserve mechanism rather than the absence of pathology.
Maintaining rich social connections, continuing to learn new skills, engaging in intellectually challenging work, and pursuing cognitively demanding hobbies are not merely quality-of-life recommendations — they are among the most effective cognitive reserve building strategies available, operating through the use-dependent synaptic density and network complexity that constitutes the brain’s resilience to pathological damage.
Free Download
Get the 7-Day Brain Optimization Protocol
The evidence-based diet, sleep, and supplement framework for your first week of cognitive enhancement — completely free.
Join 2,000+ readers optimizing their cognitive performance. Unsubscribe anytime.
Part 2: The Neuroprotective Supplementation Stack
The supplementation layer for cognitive decline prevention targets the specific neurobiological mechanisms that the lifestyle interventions leave partially unaddressed — particularly the structural neuroplasticity support, direct antioxidant neuroprotection, and neuroinflammation reduction that require dedicated nutritional or botanical compounds to optimize.
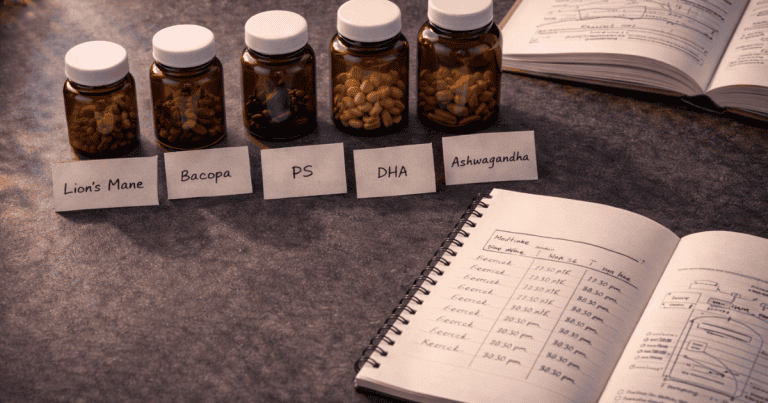
Lion’s Mane Mushroom — The NGF-Driven Structural Insurance
Lion’s Mane at 500–1,000mg daily provides the most direct available supplementation support for the NGF-driven structural neuroplasticity that cognitive reserve building depends on. By stimulating NGF production through hericenones and erinacines, Lion’s Mane supports the dendritic branching, myelination, and synaptic maintenance that constitute the physical substrate of cognitive reserve — working on a 8–16 week structural timeline that requires consistent long-term use. Clinical research by Mori and colleagues found significant improvements in cognitive function scores in older adults with mild cognitive impairment after 16 weeks of Lion’s Mane supplementation — with the improvements reversing after discontinuation, confirming the active compound mechanism rather than placebo effect.
DHA — Non-Negotiable Neuronal Membrane Health
DHA at 1,000–2,000mg daily is the nutritional foundation of cognitive decline prevention that no amount of more targeted supplementation compensates for when absent. As the primary structural lipid of neuronal membranes and the key determinant of membrane fluidity, receptor density, and synaptic signaling efficiency, DHA deficiency directly accelerates the membrane health deterioration, neuroinflammation, and hippocampal neurogenesis reduction that drive cognitive aging. Epidemiological research consistently finds that higher dietary and plasma DHA levels associate with reduced dementia risk and slower cognitive aging — with the mechanism involving both direct membrane health and the anti-inflammatory prostaglandin balance that adequate DHA maintains against omega-6-driven neuroinflammation.
Phosphatidylserine — The FDA-Recognized Cognitive Aging Intervention
Phosphatidylserine at 100–300mg daily carries the distinction of holding the only FDA qualified health claim for cognitive decline risk reduction of any supplement compound — reflecting a body of clinical evidence for its role in maintaining neuronal membrane health and receptor function across aging. PS supports the phospholipid composition of neuronal membranes that determines the density and sensitivity of neurotransmitter receptors — with age-associated PS depletion contributing to the progressive receptor sensitivity decline that underlies many age-related cognitive changes. Its cortisol-modulating effects additionally protect against the glucocorticoid hippocampal damage mechanism, providing a secondary neuroprotective function alongside its membrane health effects.
Bacopa Monnieri — Antioxidant Protection and Cholinergic Maintenance
Bacopa at 300mg daily provides direct antioxidant neuroprotection through its bacoside compounds — reducing the oxidative stress that accumulates in aging neurons and contributes to the progressive neuronal damage underlying cognitive decline. Its cholinergic enhancement effects are particularly relevant for Alzheimer’s prevention: the cholinergic system — the brain’s acetylcholine signaling network — is among the earliest and most severely affected systems in Alzheimer’s pathology, and maintaining cholinergic tone through the midlife decades of presymptomatic accumulation is a mechanistically sound preventive strategy.
Ashwagandha KSM-66 — HPA Normalization and Hippocampal Protection
Ashwagandha at 300–600mg evening dose addresses the chronic cortisol elevation that is simultaneously the most damaging modifiable contributor to hippocampal structure and the most commonly unaddressed one. For individuals experiencing chronic stress — which describes most cognitively active adults in modern environments — Ashwagandha’s HPA normalization provides direct, evidence-based protection against the glucocorticoid hippocampal damage mechanism that decades of elevated cortisol would otherwise produce.
Part 3: The Integrated Prevention Protocol — Daily Application
🛡️ Daily Cognitive Decline Prevention Protocol
MORNING
30 min moderate aerobic exercise (BDNF, hippocampal neurogenesis, amyloid clearance via improved sleep pressure) → 15–20 min mindfulness practice (HPA normalization, cortical thickness) → Morning light 30–60 min (circadian entrainment) → Supplements: Lion’s Mane 500–1,000mg + DHA 1,000–2,000mg + Bacopa 300mg + PS 100–300mg with breakfast
THROUGHOUT THE DAY
Cognitively challenging work (use-dependent synaptic density, cognitive reserve building) → Social engagement (cognitive reserve, inflammatory modulation) → Anti-inflammatory nutrition: DHA-rich foods, polyphenol-rich vegetables, low glycemic index → Caffeine cutoff by noon (adenosine preservation, SWS protection)
EVENING
Dim lighting 90 min before bed (circadian melatonin, SWS timing) → Supplements: MgT 500–1,000mg + Ashwagandha 300–600mg + L-theanine 200–400mg → Consistent 7–9h sleep window (glymphatic amyloid clearance, hippocampal neurogenesis, synaptic consolidation)
The Timeline That Matters: Years, Not Weeks
Cognitive decline prevention is a decades-long investment — which means its returns are not visible in the short term and its costs are paid by the future self rather than the present one. The 45-year-old who establishes the complete prevention protocol described in this guide is not going to feel dramatically different next month. They are making deposits into a neurobiological account that will determine whether their cognitive function at 75 resembles their function at 55 or their function at 65.
The research on lifestyle and dementia risk reduction is consistent in showing that protective effects compound with years of application. Individuals who maintain aerobic fitness across midlife show better outcomes than those who begin later. The cognitive reserve built through decades of learning is more protective than reserve built quickly in later years. The amyloid clearance benefit of consistently adequate sleep across the 40s and 50s cannot be fully compensated for by improved sleep beginning at 65. This is the honest temporal arithmetic of prevention — and understanding it is what makes starting sooner rather than waiting for symptoms the most rational possible response to the evidence.
Frequently Asked Questions About Cognitive Decline Prevention
Can cognitive decline really be prevented?
The evidence strongly supports that a significant proportion of age-related cognitive decline and dementia is preventable through modifiable lifestyle factors. The Lancet Commission on Dementia Prevention estimated that approximately 40% of dementia cases are attributable to modifiable risk factors — meaning that addressing those factors could potentially prevent or significantly delay nearly half of all dementia cases globally. For normal age-related cognitive slowing (distinct from dementia), the evidence is even more supportive of prevention and partial reversal: individuals who maintain aerobic fitness, anti-inflammatory nutrition, adequate sleep, and continuous cognitive engagement across midlife show dramatically better cognitive aging trajectories than those who do not. What cannot be prevented with current evidence is genetic deterministic risk from rare early-onset Alzheimer’s mutations — but these account for less than 5% of all cases. For the vast majority of people, cognitive decline is significantly influenced by modifiable factors, making prevention both plausible and actionable.
What foods prevent cognitive decline?
The dietary pattern most consistently associated with reduced cognitive decline risk in the research is the MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay), which Morris and colleagues found associated with a 53% reduction in Alzheimer’s risk in the highest compliance group. The MIND diet emphasizes: leafy green vegetables (daily — the strongest single food category association with reduced cognitive decline, likely through folate, vitamin K, and polyphenol content), other vegetables, berries (particularly blueberries and strawberries — the flavonoid compounds directly reduce neuroinflammation and support BDNF), whole grains, fish (weekly — the primary dietary DHA source and the single most important nutrient for neuronal membrane health and anti-inflammatory prostaglandin balance), olive oil as primary fat (oleocanthal has direct anti-neuroinflammatory properties), and nuts. The foods most strongly associated with increased cognitive decline risk are ultra-processed foods (gut dysbiosis, neuroinflammation), red meat in excess, butter and margarine, cheese, pastries, and fried food — all sharing the mechanisms of increased neuroinflammatory load, advanced glycation end product accumulation, or vascular risk factor elevation.
Does exercise prevent Alzheimer’s disease?
The evidence that regular aerobic exercise reduces Alzheimer’s disease risk is among the strongest available for any single modifiable factor. Prospective epidemiological studies consistently find that individuals who maintain regular moderate physical activity across midlife show 30–40% lower dementia incidence compared to sedentary peers. Mechanistically, the protective effects operate through multiple pathways: BDNF elevation driving hippocampal neurogenesis and synaptic density maintenance (building the cognitive reserve that delays symptom onset), direct amyloid-beta reduction through enhanced glymphatic clearance and reduced amyloid production, reduction of neuroinflammatory cytokines, improved cerebrovascular function and blood-brain barrier integrity, and reduction of the cardiovascular risk factors (hypertension, insulin resistance, obesity) that are independent dementia risk factors. Erickson’s research demonstrated the most direct evidence: older adults who began aerobic exercise showed measurable hippocampal volume increases and improved memory — a literal structural reversal of the brain aging trajectory that sedentary behavior produces. Exercise does not guarantee prevention of Alzheimer’s, but it is the most evidence-supported single lifestyle intervention for reducing its risk, and its protective effects begin accumulating from the first session and compound across years of consistency.
At what age does cognitive decline typically begin?
The neurobiological changes underlying cognitive aging begin earlier than most people expect. Hippocampal volume begins declining gradually in the 30s, with the rate of decline accelerating in the 40s and 50s in individuals with chronic stress, physical inactivity, or poor sleep. Amyloid-beta accumulation can begin as early as the 40s in individuals on a trajectory toward Alzheimer’s — 15–20 years before symptoms emerge. Processing speed, which peaks in the mid-20s and declines gradually thereafter, shows measurable slowing beginning in the mid-30s under laboratory conditions. Working memory capacity begins to show age-related changes in the 40s that become more significant through the 50s. The cognitive functions most resistant to early aging are vocabulary, general knowledge, and accumulated expertise, which typically remain stable or improve through the 60s. The practical implication is that the 40s and 50s are the highest-leverage decade for preventive intervention — the period when pathological processes are underway but cognitive reserve is still largely intact, making the behavioral investments of this guide most cost-effective per year of application.
Prevention as the Only Strategy That Works
The pharmaceutical approach to Alzheimer’s disease — decades of drug development targeting amyloid-beta after clinical diagnosis — has produced a failure rate exceeding 99% in clinical trials, with the rare successful drugs producing modest symptomatic benefits rather than disease reversal. The biology explains why: by the time clinical symptoms emerge, the pathological cascade has been underway for 15–20 years, the neuronal loss is substantial, and the intervention window for meaningful structural reversal has largely closed.
Prevention — applied in the decades before symptoms — is not merely the best available strategy for cognitive health. It is the only strategy that the biology supports with compelling evidence. The interventions in this guide are not exotic or expensive. Aerobic exercise, adequate sleep, anti-inflammatory nutrition, stress management, social engagement, continuous learning, and the supplementation compounds that directly support the molecular mechanisms of neuroprotection are accessible, evidence-based, and profoundly effective when applied consistently across the decades that determine cognitive fate.
The most important thing to understand about cognitive decline prevention is that the best time to begin was 20 years ago and the second-best time is now — not because starting later is futile, but because the neuroplasticity that makes the brain responsive to these interventions operates at every age, and each year of consistent application adds to the cognitive reserve that determines outcomes decades forward.
For the complete neuroscience of the mechanisms addressed by this protocol, see the brain health guide and neuroplasticity guide. For the nootropics that provide supplementation neuroprotection, see the nootropics for brain health guide. For the anti-inflammatory dietary protocols, see the anti-inflammatory diet guide.
References
- Livingston, G., et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413–446. PubMed
- Erickson, K.I., et al. (2011). Exercise training increases size of hippocampus and improves memory. PNAS, 108(7), 3017–3022. PubMed
- Morris, M.C., et al. (2015). MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimer’s & Dementia, 11(9), 1007–1014. PubMed
- Lucey, B.P., et al. (2019). Effect of sleep on overnight CSF amyloid-β kinetics. Annals of Neurology, 85(2), 197–205. PubMed
- Stern, Y. (2012). Cognitive reserve in ageing and Alzheimer’s disease. The Lancet Neurology, 11(11), 1006–1012. PubMed
- Mori, K., et al. (2009). Improving effects of Yamabushitake on mild cognitive impairment. Phytotherapy Research, 23(3), 367–372. PubMed
- Kivimäki, M., et al. (2012). Job strain as a risk factor for coronary heart disease: A collaborative meta-analysis of individual participant data. The Lancet, 380(9852), 1491–1497. PubMed
- Hölzel, B.K., et al. (2011). Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Research: Neuroimaging, 191(1), 36–43. PubMed
- Xie, L., et al. (2013). Sleep drives metabolite clearance from the adult brain. Science, 342(6156), 373–377. PubMed
- Cotman, C.W., & Berchtold, N.C. (2002). Exercise: A behavioral intervention to enhance brain health and plasticity. Trends in Neurosciences, 25(6), 295–301. PubMed
Tags: how to prevent cognitive decline, cognitive decline prevention, prevent Alzheimer’s disease, dementia prevention, brain health aging, Lancet Commission dementia, MIND diet brain health, exercise Alzheimer’s prevention, sleep cognitive decline, hippocampal neurogenesis aging, cognitive reserve dementia, Lion’s Mane cognitive decline, DHA dementia prevention, glymphatic amyloid clearance, neuroprotection protocol
About Peter Benson
Peter Benson is a cognitive enhancement researcher and certified mindfulness coach with 18+ years of personal and professional experience in nootropics, neuroplasticity, and brain health optimization. He has personally coached hundreds of individuals through integrated cognitive performance programs combining evidence-based lifestyle protocols with targeted supplementation. NeuroEdge Formula is his platform for sharing rigorous, safety-first cognitive enhancement guidance.